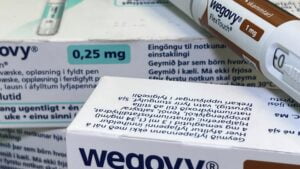
The U.S. has witnessed a groundbreaking shift in the use of a popular weight loss drug, Wegovy. Originally prescribed for weight loss, Wegovy has now been approved for heart health as well. However, despite this expanded approval, many insurance plans are hesitant to cover the drug due to its high monthly cost of $1,350.
Insurance experts predict that some plans may reconsider covering Wegovy in the future as they update their formularies, but challenges remain. With approximately 110 million American adults living with obesity, and only around 50 million having insurance coverage for weight loss drugs, there is a substantial gap in coverage.
The recent approval of Wegovy for heart health highlights the potential downstream health benefits of weight loss drugs, challenging the notion that they only offer cosmetic benefits. Health experts argue that covering these medications could lead to long-term cost savings and improved health outcomes for patients.
Despite these potential benefits, some employers are hesitant to cover weight loss drugs due to concerns about long-term data and costs. For example, the state of North Carolina recently announced it would no longer cover GLP-1s for weight loss due to financial concerns.
As discussions around coverage and costs continue, it is clear that there are still obstacles to overcome in providing access to effective weight loss treatments. However, increased competition in the market and the development of more affordable options could pave the way for broader coverage in the future. In the meantime, employers and insurers will need to carefully consider how to balance coverage with cost controls to ensure access to these important treatments.
Source link