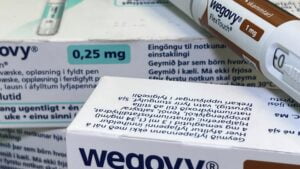
The U.S. has seen a surge in popularity for weight loss treatments, particularly Wegovy. This blockbuster drug, known for its effectiveness in weight loss, has now been approved for heart health as well. However, broader insurance coverage for this weekly injection drug from Novo Nordisk and similar obesity treatments is not yet guaranteed.
Many employers and health plans are hesitant to cover Wegovy due to its high monthly cost of $1,350, which they fear could strain their budgets. Additionally, there are concerns about the duration of treatment and how long patients stay on the drug. Despite these challenges, some insurance industry experts believe that with Wegovy’s new approval, plans may start considering coverage when they update their formularies in the future.
The coverage for GLP-1 drugs, like Wegovy, for weight loss remains inconsistent. Approximately 50 million American adults with obesity have insurance coverage for weight loss drugs, but there is a push for broader coverage from private insurers, employers, and the federal Medicare program.
The recent FDA approval of Wegovy for heart management highlights the downstream health benefits of the drug and similar treatments for severe conditions related to excess weight. This approval challenges the outdated notion that weight loss treatments only offer cosmetic benefits, shifting the conversation towards its life-saving potential.
However, the high costs associated with covering Wegovy and other GLP-1s are a major concern, leading some states, like North Carolina, to scale back coverage. Despite efforts to negotiate costs with drugmakers like Novo Nordisk and Eli Lilly, challenges remain in finding a balance between providing access to these treatments and managing costs effectively.
As employers and health plans navigate the complexities of covering weight loss drugs, strategies such as implementing cost controls and requirements may be crucial. By setting limits on spending increases and exploring alternative options like oral versions of these drugs, there is hope for a more inclusive and sustainable approach to coverage in the future.
Source link